 “The backlog in elective surgery has very little to do with the COVID-19 pandemic and almost everything to do with savage cuts to the ACT health budget by the ALP and the Greens over the last six years,” writes columnist JON STANHOPE.
“The backlog in elective surgery has very little to do with the COVID-19 pandemic and almost everything to do with savage cuts to the ACT health budget by the ALP and the Greens over the last six years,” writes columnist JON STANHOPE.
ACT Health Minister Rachel Stephen-Smith recently announced a funding boost of $30 million to tackle what she characterised as the backlog in elective surgery due to the COVID-19 pandemic.

Elective surgery was paused for just on four weeks from the end of March to the end of April.
Health CEO Bernadette McDonald was also quoted as saying that there would, by July 1, be about 2250 surgeries that had been planned but that would not be performed.
Ms McDonald identified these as “planned” surgeries so one assumes that ACT Health had been fully funded to carry them out.
It follows, therefore, that since these “planned” surgeries were not performed that most of the allocated funding should still be in the bank waiting to be spent.
The reality is, of course, as we all know but out of an apparent surfeit of politeness or because we really don’t care, are loath to say, the backlog in elective surgery in the ACT has very little to do with the COVID-19 pandemic and almost everything to do with a series of savage cuts to the ACT health budget by the ALP and the Greens over the last six years.
My colleague Dr Khalid Ahmed and I have recently looked again at the waiting times for elective surgery in public hospitals in Australia.
 While it is true that waiting times have increased across Australia over the last six years, the increase in the ACT has outstripped all other jurisdictions and is significantly higher than the national average.
While it is true that waiting times have increased across Australia over the last six years, the increase in the ACT has outstripped all other jurisdictions and is significantly higher than the national average.
We have outlined in detail the findings of our latest review of elective surgery in a blog posted to the University of Canberra Policy Space.
A summary of some of our findings are:
- A comparison of the median waiting time in the number of days for half of all patients from 2014-15 to 2018-19 reveals that in aggregate ACT patients waited 17 per cent to 62 per cent longer than patients at the national average.
- In relation to orthopaedic surgery the median wait time in the ACT was 55 per cent longer than the average in like (peer) hospitals across Australia. The number of Canberra residents who waited longer than 365 days for orthopaedic surgery in a public hospital was proportionately four times higher than the national average.
- In relation to gynaecological surgery the ACT’s performance was much worse than its peer group of public hospitals and in fact the second worst in Australia. The median wait time for a Canberra woman, without private health insurance, requiring surgery for a gynaecological issue was 32 per cent higher than the peer average. The number of Canberra women who waited longer than 365 days for such surgery, in a public hospital, was proportionately a staggering 425 per cent of the Australian average.
The Australian Institute for Health and Welfare has reported that between 2014-15 and 2018-19 admissions for elective surgery in the ACT increased at an annual rate of 4.2 per cent. This was driven by annual growth of 2.2 per cent in admissions per 1000 population, with the remainder attributable to population growth.
There are a number of acknowledged drivers of demand for health care such as the ageing of the population, changes in technology and inflation in the cost of wages and medicines.
The Productivity Commission has indicated that the impact of these factors on the rate of utilisation growth in the ACT is 3.2 per cent.
Despite the incremental increase in per person demand for health care the ACT government has for a number of years reduced funding for health by 1 per cent per annum in real terms. A reduction of 1 per cent equates to more than $100 million a year.
These cuts are unavoidably reflected in the funding allocated for elective surgery. If the demand growth parameters referred to above were accounted for, then Dr Ahmed and I calculate that there would, conservatively, have been an additional 1400 admissions for elective surgery in the last three years, exclusive of the backlog that existed before that.
To be blunt the $30 million, one off, sugar hit announced by Minister Stephen-Smith will have no impact on elective surgery waiting times beyond this (election) year.
Public hospitals are responsible for about one third of elective surgery performed in Australia. Patients on the public waiting list typically have no health insurance with hospital cover, or if they do have such cover, they are unable to afford out-of-pocket costs in a private hospital.
Those of us who can afford private health insurance have guaranteed timely access to health care. Those Canberrans who cannot afford to pay, most typically pensioners, the working poor and people otherwise from low-income households must wait – often in pain, misery and uncertainty. Access to health care in Canberra is increasingly determined by capacity to pay rather than need.
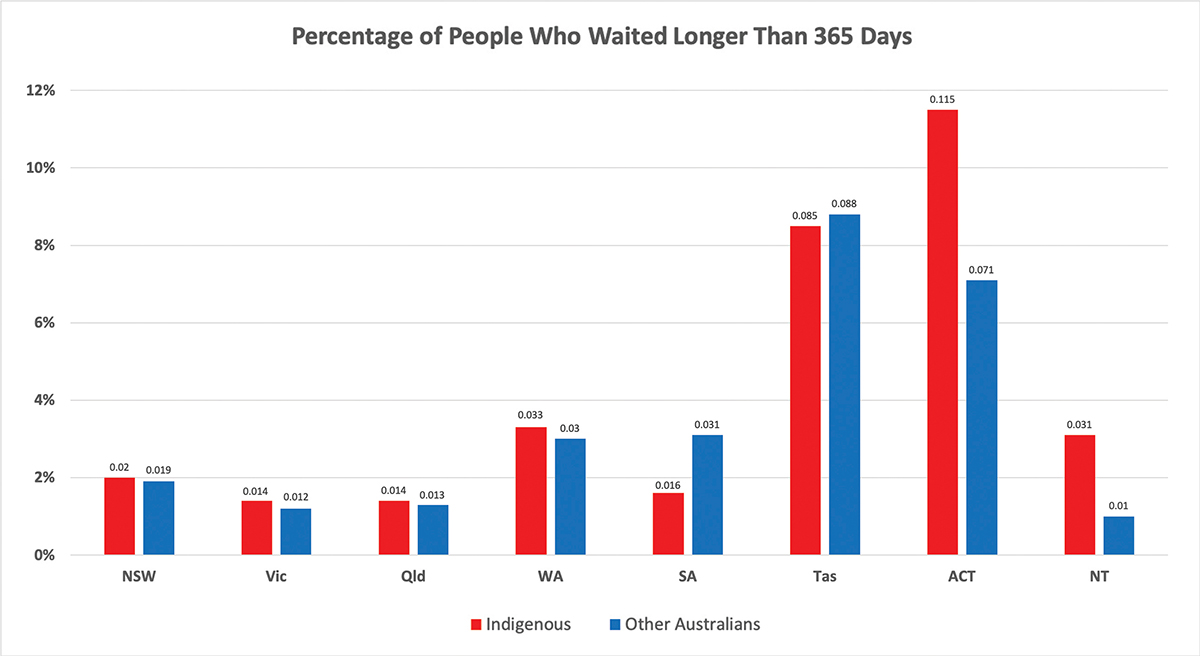
Dr Ahmed and I have previously written about the extent to which the extent of the rationing of health services by the ACT government inevitably leads to the entrenching of major distributional inequities in associated service delivery systems. The chart above, which compares by Aboriginal status, the percentage of people in Australia who waited longer than 365 days for elective surgery, in 2018-19, validates our concerns.
Who can be trusted?
In a world of spin and confusion, there’s never been a more important time to support independent journalism in Canberra.
If you trust our work online and want to enforce the power of independent voices, I invite you to make a small contribution.
Every dollar of support is invested back into our journalism to help keep citynews.com.au strong and free.
Thank you,
Ian Meikle, editor






Leave a Reply