By Rachael Ward in Melbourne
When Jane Fletcher went into hospital for routine surgery she never expected to come out with a superbug and a front-row seat to the ‘silent pandemic’.
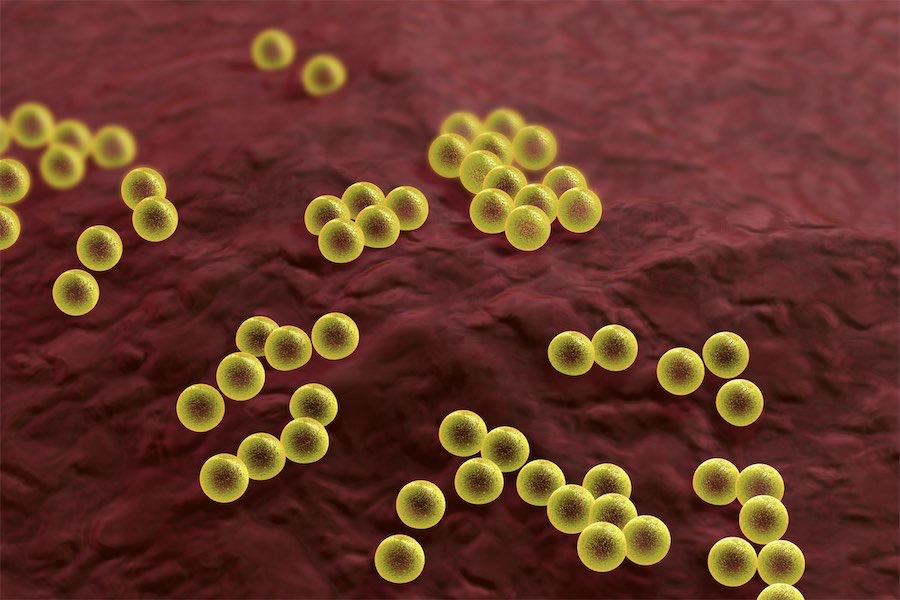
The health psychologist was struck down with antibiotic-resistant golden staph and joined the ranks of an estimated tens of thousands of Australians infected with bacteria, viruses, fungi and parasites that don’t respond to medicine each year.
“It’s quite petrifying, really,” Ms Fletcher told AAP.
The 56-year-old has been immunocompromised since having a double lung transplant and said she’s used to all sorts of infections, but living with the superbug commonly referred to as MRSA has been something else.
“Once you have a superbug you have a superbug, that never goes away and that is a label that stays with you forever,” she said.
Some 10 million people globally are expected to die from antimicrobial resistance each year by 2050, as the pipeline of new treatments dries up and existing medications struggle to stay on top of changes to bugs over time.
“It’s probably quite likely that we will come to the end of the antibiotic era in the coming decades, unless there are significant new scientific advances,” microbiologist and infectious diseases physician Associate Professor Norelle Sherry told AAP.
“Antimicrobial resistance, or AMR, is a huge silent pandemic that is not talked about enough globally or here in Australia.
“We’re seeing increasing rates of antibiotic resistance in bacteria that really threaten human health.”
The scientist from the World Health Organisation’s Collaborating Centre for Antimicrobial Resistance at the Doherty Institute said superbugs acquired overseas in the broader Asia-Pacific region, such as a drug-resistant strain of gonorrhoea, are a huge threat to national health security.
She said the remaining ‘last resort’ antibiotics are used sparingly due to worse side effects, the huge costs to the health system and fears they, too, won’t work soon.
“We are literally getting to the stage where there are very few or no antibiotics that we can treat patients with and this is, this is the potential disaster that we are all very concerned about,” Associate Professor Norelle Sherry said.
An urgent need for further data collection on superbugs was highlighted in national strategies to fight resistance in both humans and animals, on top of a significant focus on clinicians using medications wisely.
Many infectious diseases specialists and some pharmaceutical companies also want Australia to adopt a UK subscription-style funding model to encourage drug companies to pour more money into developing new treatments.
“A country pays for access to one of these last one antibiotics, so that the drug companies can still afford to do the very expensive discovery work,” Prof Sherry explained.
That’s because the market for research and development on antimicrobials is “broken”, according to Pfizer Australia and New Zealand’s managing director Anne Harris.
She said under normal circumstances medications cost $2 billion to develop and years of common usage before they make money, but antimicrobial medicines are different as they can only be used sparingly.
“What it means is you never get the return back on your research, development, manufacturing et cetera and so what is really going to be required … is to have more novel ways of funding antimicrobials,” she said.
The pharmaceutical giant this week revealed a $150 million upgrade to its Mulgrave manufacturing plant to boost production of its antimicrobials in Australia by 30 per cent from 2026, with drugs expected to be used in 60 countries.
Federal authorities are looking at different funding models overseas and the government is considering a range of possibilities as part of a wider health review but is yet to respond, a spokesperson for the Department of Health and Aged Care said.
“It is currently too soon to evaluate how impactful these (subscriptions) models are at stimulating research, development and innovation in antimicrobials,” they said.
An additional $22.3 million is being spent over the next four years on the Antimicrobial Use and Resistance in Australia surveillance program, with findings guiding action on any misuse.
Australian Veterinary Association board member and former Chief Veterinary Health Officer Mark Schipp said the majority of all antimicrobial medicines are used in livestock, although so far superbugs aren’t common in animals.
Fortunately, most of Australia’s livestock is raised in open air paddocks rather than cramped barns, where animals are prone to infections, although acknowledged commercial pressures can come into play from industry.
“Certainly there can be a tension, but the role of the veterinarian is to look out for the best interests of the animal and the way to do that is to try and prevent infection in the first place,” he said.
When superbugs are seen in animals, it’s usually pets living with their owners.
“Often they’re very similar infections to what you would expect to see in humans, so skin infections and the like,” he said.
“On occasion, it is that the owner and the animal share infections or share resistances.”
The Royal Australian College of General Practitioners has pushed back against pharmacist-prescribing trials in several states for limited ailments like urinary tract infections, over concerns it could promote resistance.
The college’s Acting Vice President Dr Ramya Raman said wide-spectrum antibiotics are still valuable under the right conditions but urged patients to listen to their GP if they do not recommend medication.
She said many people misunderstand how some conditions are treated and seek out pills for respiratory, gastrointestinal and urinary infections.
“We’ve got to keep the longer perspective, because if a treatment or a medication is actually not going to be helpful in managing that condition, there’s really no use in taking the antibiotic, because it might actually just cause unnecessary side effects,” she said.
So far Ms Fletcher has responded well to treatment for her golden staph but still urged Australians to be vigilant.
In an effort to reduce the spread, patients with superbugs are isolated, subjected to strict infection control and put last on surgery lists.
“My ability to have an operation in many hospitals is still compromised because I’ll be last on the list because I’ve had MRSA in recent times,” she said.
Ms Fletcher does not believe there should be more restrictions on prescribing antibiotics but stressed everyone has a role to play, including members of the public who should keep up good hygiene habits like hand washing.
“It has to be a community, a government and a big pharma approach,” she said.
“We have the possibility for people like me to be able to have a stress-free life and not be worried about what new superbugs around the corner,” she said.
Who can be trusted?
In a world of spin and confusion, there’s never been a more important time to support independent journalism in Canberra.
If you trust our work online and want to enforce the power of independent voices, I invite you to make a small contribution.
Every dollar of support is invested back into our journalism to help keep citynews.com.au strong and free.
Thank you,
Ian Meikle, editor





Leave a Reply